Possible Links between Blood Types and Covid-19 Infection by Lorelai Brunner; Animas High School (Durango, CO) on Scribd

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License.
Possible Links between Blood Types and Covid-19 Infection by Lorelai Brunner; Animas High School (Durango, CO) on Scribd

By Ross Echols; Farnsley Middle School (Louisville, KY)
In the summer of 1988, my father, Darrel Echols was rushed to the hospital due to chest pains. In an interview, he said, “My chest felt tight and I was a little short of breath.” He was later diagnosed with mitral valve prolapse. At the time, he was 19.
According to WebMD and the American Heart Association, mitral valve prolapse (MVP) is when the mitral valve leaflets bend backwards into the left atrium as the left ventricle contracts. So think of the mitral valve as a gate between two parts of your heart. Blood goes through the valve. Normally, the blood flows through one way and doesn’t go
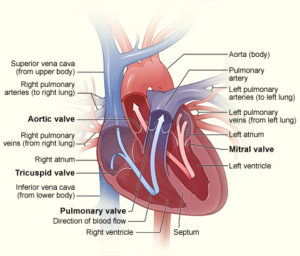
back the other way. A “leaky” mitral valve means that blood can go back through he mitral valve, known as mitral regurgitation.
According to the American Heart Association, MVP can occur due to being born with a genetic risk of developing into MVP, having abnormally stretchy mitral valve leaflets, or some connective tissue disorders. Mitral valve prolapse isn’t very common, it only occurs in seven percent of the population, mostly women, and it is known to run in families. Serious symptoms tend to occur in men older than age fifty.
According to the Mayo Clinic, doctors may use an echocardiogram (ECG), a stress test, or a coronary angiogram to diagnose MVP. An echocardiogram is machine that has probes that are placed on the chest to record the impulses that cause the heart to beat. A stress test is where a doctor has a patient exercise or take medications to increase heart rate to check for mitral regurgitation. Mitral regurgitation is when the heart pumps blood from the left atrium through the mitral valve into the left ventricle, some of the blood leaks back into the left atrium. Atriums and ventricles are basically four sections of the heart. There are also the right atrium and ventricle, and separating them is the tricuspid valve. Cardiologists can also use x-rays of the chest to diagnose mitral valve prolapse. Echols was diagnosed using an ECG, ultrasound of the heart, and a heart monitor.
Dr. Wayne Gibson, a professor of cardiology who works in Jeffersonville, IN stated in an office visit with Echols that symptoms include shortness of breath, chest pain, and skipped and extra heartbeats. He also said that there is a treatment known as a beta blocker that can slow one’s heart rate and prevent extra beats. Most medications for mitral valve prolapse only treat the symptoms, as do beta blockers. Ninety percent of people diagnosed with mitral valve prolapse will not need surgery to correct it. If needed, surgeons can implant an artificial valve. “I suffer from chest pains, shortness of breath, and accelerated heart rate,” Echols says.
According to MVP Resource, most people with MVP should avoid food and drink with caffeine and other stimulants (i.e. coffee, tea, chocolate, etc) because it stimulates the autonomic nervous system (ANS), causing it to become unstable. “When the ANS becomes unstable, body functions slow down or speed up inappropriately. This can have a significant effect on MVP symptoms.” MVP Resource also says you should avoid sweets/candy, soft drinks, alcohol, and fruit juice. Echols avoids pretty much anything with caffeine.
Echols is doing fine now. He states, “Even though I’ll probably have mitral valve prolapse for the rest of my life, I won’t let it get in the way of spending time with my wife and kids.”

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License.

By Maggie Marshall and Cheyenne Reynolds; Farnsley Middle School (Louisville, Ky)
“It all started when Maggie was around 6 months old. She was always crying or sleeping; usually she was crying,” says Billie Marshall, Maggie’s mother. “Whenever she had a ‘flare up’ she would get small red bumps/spots. It would usually only be one or two spots. We didn’t really know how to act, we didn’t know what it was. We think she got it from her grandmother since she was a nurse at a hospital.”
Maggie’s parents found out she had MRSA because one day they took her to the family pediatrician because they thought she had a cold. After they found that out, Maggie’s parents started taking her to that doctor and they prescribed her stronger antibiotics. Her MRSA flare ups finally ended when she was around 2 years old.
Methicillin-resistant Staphylococcus aureus (MRSA) is an infection that can be mild, but it can evolve to be very deadly! According to WebMD, MRSA is bacterium that causes infections in many parts of the body. It is resistant to most antibiotics, so it makes it very difficult to treat. MRSA makes small red bumps on the skin that may irritate, depending on how bad the infection is. It usually affects only young people or older people because they have lower immune systems which makes them more susceptible to infection.
The Centers for Disease Control and Prevention (CDC) talks about MRSA being the cause of most skin infections. Sometimes it can cause pneumonia and other problems. You can get sepsis (a life-threatening reaction to severe infection in the body) if the MRSA infection is left untreated.
The CDC did a study that shows one in three people carry staph MRSA in their nose, but it usually doesn’t carry the illness. The amount of MRSA infections in healthcare facilities are declining. Between 2005 and 2011, invasive MRSA infections that began in hospitals declined 54%, with 30,800 fewer severe MRSA infections. Also, the study showed there were 9,000 fewer deaths from MRSA in hospital patients in 2011 versus in 2005.
National Center for Biology Information (NCBI) says that MRSA can be community-associated MRSA (CA-MRSA) and hospital acquired MRSA (HA-MRSA). “You can get CA-MRSA from touching another person that has it on their skin. Someone can get HA-MRSA from being in a hospital or a healthcare facility.”
CA-MRSA can cause infections on the skin that might look like a pimple/boil. “If the infection is left untreated it may develop into serious, life-threatening issues such as infections in the bloodstream, bones, joints, or lungs. Although it is less likely, you can get MRSA in other parts of the body like lungs, bloods, eyes, and urine,” says Medicine Net.
Medicine Net says MRSA has many different symptoms for the different types. “Symptoms of MRSA are: large, red, painful bumps under the skin (boils), small sores that look and feel like spider bites.” The boils/pimples that form are normally hot and filled with pus. “More symptoms are: headache, generally feeling sick, muscle aches, shortness of breath, fatigue fever, shivering, coughing, and chest pain.”
Medicine Net states “Since the 1960s, MRSA has picked up more resistance to different antibiotics. Overuse of antibiotics has increased resistance in MRSA and other infectious bacteria, because resistance genes (the genes that code for resistance) can be passed from bacteria to bacteria.”
According to Mayo Clinic, since MRSA is an infection that is very resistant, it is hard to treat it. Usually, doctors will prescribe antibiotics that will control the infection. Since it’s so hard to get rid of it you have to keep your skin very clean. The boils/pimples will look like they need to be popped, but do not squeeze, poke, or pop the boil. If you pop it the pus inside will spread and make more boils/pimples to form.
To prevent from getting MRSA Mayo Clinic says “Wash your hands. Careful hand washing remains your best defense against germs. Scrub hands briskly for at least 15 seconds, then dry them with a disposable towel and use another towel to turn off the faucet.” For extra cleanliness you could carry a small bottle of hand sanitizer that has at least 62% alcohol for times when you don’t have access to soap and water. You would also want to keep wounds covered, keep cuts and wounds clean and covered with dry bandages until they heal. The pus from infected sores may contain MRSA, and keeping wounds covered will help prevent the infection from spreading.
Indiana University of Pennsylvania says you would also want to keep personal items personal for example, avoid sharing personal items such as towels, sheets, razors, clothing and athletic equipment. “MRSA spreads on contaminated objects as well as through direct contact.” Always shower after athletic games or practices. “Shower immediately after each game or practice. Use soap and water. Don’t share towels. Sanitize linens.” If you have a cut or sore, wash towels and bed sheets in a washing machine set to the hottest water setting (with added bleach, if possible) and dry them in a hot dryer. Wash gym and athletic clothes after you wear them.
It’s been about 11 years since Maggie last had a flare up and MRSA has not affected her since then. “I’m glad the flare ups ended when they did, I would hate to still be struggling with that infection,” says Maggie.

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License.

By Rayna Randers and Katy Cano; Farnsley Middle School (Louisville, KY)
When Katy (co-author) was born, her parents noticed a little red dot below her left eye. They thought it would eventually go away. However, the red dot didn’t go away and it kept getting bigger, up to half of her face causing her not to be able to see out of her left eye.
Katy’s parents, Aura Aguilar and Clementino Cano, states “We were worried so we took her to the hospital. We wanted to know what was happening to her face.”
Katy’s doctor diagnosed her with hemangioma. According to the Mayo Clinic, “Hemangioma is a birthmark that commonly appears as a rubbery, bright red nodule of extra blood vessel in the skin.” Certain Hemangioma look darker than others and in some rare cases it to grows into the lower layers of the skin or in the muscle. This is called a deep lesion. In Katy’s case her lesion was only skin deep. “Hemangioma is extremely rare, 200,000 people are diagnosed each year,” stated the Mayo Clinic.
In an email to Scijourner, Leah Baker, who is part of The Disease and Vascular Malformation Team at the Cincinnati Children’s Hospital Medical Center, wrote that “In most cases a diagnosis is made by correlating medical history with a physical examination findings. In certain cases, radiological test such as Magnetic Resonance Imaging (MRI) or computed tomography may be used when trying to make a diagnosis or determining a lesion. It’s an imaging procedure that uses special x-ray equipment to create detailed pictures, or scans, of areas inside the body.”
The Mayo Clinic stated that some symptoms of hemangioma may be present at birth but more often appears during the first several months of life. It starts out as a flat red mark anywhere on the body most often on the face, scalp, chest, or back. Usually, a child has only one mark like Katy. Some children may have more than one mark particularly if they’re part of a multiple birth.
Katy’s doctors at the University of Florida Physicians requested to do laser surgery when Katy was about 3 months old. They told Katy’s parents that in some cases of hemangioma can disappeared or go away, but in Katy’s case her spot was half way across her face. Therefore, her birthmark would not have gone away.
The surgeries they recommended were done by using an extremely hot, focused beam of light that helps remove tissue and controls any bleeding from the surgery wound. Before she had the surgeries, her left eye was shut and Katy couldn’t see. Half of her face looked like a huge red balloon that was about to pop. In reality these surgeries helped her open her eye.
“We were worried that Katy would lose her eyesight,” states Katy’s parents.
According to the Hemangioma and Vascular Malformation Team, some common treatment options include drug therapy, which is a medical therapy used when the lesion is rapidly forming. Some medications include Timolol, which is a medication applied directly to the hemangioma, and corticosteroids, which can be injected into the skin or taken orally.
Complications of a hemangioma can lead to destruction of the skin and also develop a sore. This can also lead to pain and bleeding. Depending where the hemangioma is located, you may have trouble with vision, breathing, or hearing, but this usually rare.
Hemangioma is noncancerous and it really doesn’t increase your risk of getting cancer. And this tumor is usually starts smaller, but it can grow much larger.
In Katy’s case, laser surgery was needed due to her age. But there was some risk that it might result with a scar and changes in the area. Katy now has a scar underneath her left eye from all the surgeries.
“I now can see better and I am thankful to all doctors who helped me recover from Hemangioma,” says Katy. “Now I only have a scar on my left cheek and no longer have to go through surgeries”.

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License.

By Candace Cavaco; Kamehameha Schools (Kea’au, HI)
I know so many people that love spicy foods, including a lot of friends and family, but I don’t like ANYTHING with even a hint of heat. I just don’t have the taste for it. Some people even like getting a type of high off of the endorphins released when they eat spicy foods. This made me wonder if I was missing out on anything. Why don’t I care for these types of foods? Are there secret benefits from eating spicy foods? Does it help your health, can it cure cancer?
First, a little background behind why spicy foods are spicy: capsaicin is the active component in chili peppers and other hot flavors. Chili powder, paprika, and curry spices are common sources of the heat in many foods.
WebMD says capsaicin creates the burning sensation on your tongue, and it is used in creams and patches to relieve pain. So what does the capsaicin in you food do? Of course many people know that spicy foods can cause heartburn, acid reflux, gas, and many other things, but can these foods also be good for you?
A 2015 study by Harvard Medical School in Boston shows that, people with spicy diets can have a 10% decrease in chance for premature death. Fresh chili peppers are linked to easing arthritis pain, as well as lowering the risk of death by cancer, heart disease, and type two diabetes.
An article by Dr. Adam Simon on Push Doctor confirms this. This effect was shown to be even greater in people that don’t drink alcohol.
Just last year, research published in the journal PLOS One reported that including hot red chili peppers in their diet is associated with a 13% lower risk of death. The study by University of Vermont researchers involved more than 16,000 Americans.
Now, this begs the question, why do some people have a higher tolerance for heat and spicy things, and others, like me, can’t stand it? According to Science Line, your susceptibility to hot foods can be determined by your genetics and the pain receptors you are born with, and your personality could have something to do with it.
Based on research from the University of Helsinki, some people inherit fewer capsaicin receptors than others, and that gives them a higher tolerance to capsaicin and its effects. The less receptors you have, the less heat you’ll feel when tasting the food. In case you were wondering, the university also says the pain receptors in your tongue don’t necessarily have a connection with the pain tolerance of your body, so you can have a large amount of capsaicin receptors, and still have a high pain tolerance for the rest of your body.
You can also build up a tolerance for spicy foods based on your diet. For example, children raised eating foods that have a lot of heat in them, possibly because of their heritage, can develop a preference for the flavor, says John Prescott, who is an experimental psychologist, as well as the author of the book Taste Matters.
In an 2013 article published in Food Quality and Preference by researchers from Pennsylvania State University, it was reported that personality may be associated with your liking of spicy foods. It was shown that people who were outgoing and like taking risks were more inclined to like hot foods, while most people less outgoing disliked the spicy food served.
Another study done by the same researchers at Penn State University “confirmed that liking or disliking spicy foods is not only determined by one’s sensitivity to capsaicin but that personality factors do exist” and effects peoples’ reaction to tasting the food and the initial burning.
“The more irritating a compound or food gets, the less people should like it, but that’s not always the case,” said Nadia Byrnes, one of the Penn State scientists, in a news release by EurekAlert!.
Some people can even develop an addiction to spicy food, or the effect the capsaicin has on their brain, says a scientific blog by the Northwestern University research center. When tasting it, your body will sense pain and send pain receptors to your brain; this releases endorphins as well as dopamine. This reaction gives your body a sense of “high” and it makes you feel good.
Kalsec, a global producer of natural spice and herb flavor extracts, colors, and antioxidants, wrote that according to their online surveys, “90 percent of U.S. consumers and 80 percent of European consumers enjoy hot and spicy foods.”
So maybe the liking of spicy foods skipped a generation in my family, or maybe I’m not a risk taker. I’m not sure if the data from all of these studies and research is true for everyone, but for the ones that enjoy the tingling caused by eating spicy food, maybe they’ll end up living longer than I will.

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License.
By Gabriel Skaggs and Dylan Walter; Farnsley Middle School (Louisville, KY)
“It was really hard to breathe.” said Ronnie Walter, co-author Dylan’s Dad. “When I got to the hospital my doctor found out I had a pulmonary embolism, and that I was very lucky to live. That made me scared. We went to the emergency room, and they hooked up all kinds of machines up to my nose to allow me to breath.”
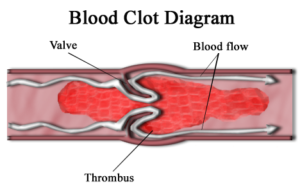
According to the Mayo Clinic, a pulmonary embolism (PE) is caused by a blood clot in the leg that becomes loose and travels to the lungs. (Pulmonary means related to the lungs. Embolism means blocking of an artery, usually by a blood clot or an air bubble.) This can be quite dangerous if not treated properly.
“The blocks can be caused by fat from marrow from a broken collagen [structural protein] or other tissue, part of a tumor, and air bubbles,” states Mayo Clinic. If you wait 3 to 4 days to get treated, there is a high chance of death.
According to WebMD, “The major symptoms are fast heart rate, shortness of breath, chest pain, and coughing a lot. There can also be leg pain, or swelling or both, usually in the calf.” If you have these symptoms you need to go to a doctor right away, your life could be in danger. About 30,000 Americans die each year from PE in the U.S.
According to Mayo Clinic, one reason for PE is Deep Vein Thrombosis (DVT blood clot). A DVT blood clot is when a blood clot gets deep in one of the veins.
Another cause of PE is inactivity, if you’re not active it could stop your blood from flowing properly.
PE can also occur when your blood doesn’t flow properly. If it pools in your heart or blood vessels, the platelets are more likely to stick together.
According to Mayo Clinic, “If one of your parents experienced PE Blood clots often, you have a higher chance to experience them than people who have had parents who did not.” Another cause is if you are hurt and sit down for a long time without any movement a clot can form and go to your lungs.
PE Blood clots have a treatment. One treatment is thrombolytic treatment, to dissolve clots with drugs. One more treatment for PE is surgery in which doctors remove the embolic—a blood clot, air bubble, piece of fatty deposit, or other object which has been carried in the bloodstream to lodge in a vessel and cause an embolism. One last treatment for Pulmonary Embolism is getting a filter put in the vena cava so it can stop any blood clots before they reach your lungs.
According to Angie Johnson, a resource teacher at Farnsley Middle School who has personal knowledge of this, if you have any type of blood clot you avoid eating foods with vitamin K, such as kale, spinach, turnip greens, swiss chard, or any green leafy vegetables. This is because vitamin K thickens the blood causing blood clots or making them worse.
After four day, Ronnie Walter got out of the hospital free of PE and mostly healthy. “Even though I was feeling weak when I got out of the hospital, I felt great. And I was just glad to not be at the hospital any longer.” Now Ronnie Walter does not have PE anymore, although he has a higher risk of getting it again than most.

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License.

By Kayla Nguyen; Farnsley Middle School (Louisville, KY)
My mom first noticed my eczema when I was about 6 years old. She noticed I kept scratching my inner elbow and how dry it was. She told my Dad, and he took me to the doctor. There, the doctor diagnosed me with atopic dermatitis.
According to the Mayo Clinic, “Atopic dermatitis is a condition that makes your skin red and itchy.” The more common name for atopic dermatitis is eczema.
Dermatitis, as stated by Wikipedia, “…is a group of diseases that results in inflammation of the skin.”
According to Sharecare, a health and wellness engagement platform, about 10% to 20% percent of children and about 3% of adults are diagnosed with eczema in the US. Your family doctor can diagnose eczema.
People with atopic dermatitis tend to develop the condition before the age of five and about half grow out of the symptoms as they get older.
Some symptoms of eczema are itch; redness; pain; inflammation; rash; and dry, scaly skin. According to the National Eczema Association (NEA), “Eczema flares are frequently triggered by the itch-scratch cycle.” The “itch-scratch cycle” is when itching leads to scratching, which ends in the release of inflammatory mediators—molecules that are released by immune cells during times when harmful agents invade our body—and therefore leading to the growth of eczema and more dry skin.
Of these symptoms I experienced itchiness; dry, scaly skin; and redness.
According to WebMD, a health and medical news site, atopic dermatitis is the most common and the most severe type of eczema. Causes of eczema are unknown, although there are many contributing factors, such as the environment you live in or your genetics. Most people who have atopic dermatitis have a personal or family history with allergies such as hay fever (allergic rhinitis) or asthma.
My grandfather had asthma so that may have been a contributing factor to my eczema. I have neither asthma or allergies.
Since a lot of people with eczema also suffer from allergies, your doctor may refer you to allergy tests to see possible irritants or triggers. Since I did not have allergies, this is not what happened to me.
Some environmental factors that could contribute to having eczema, according to the Hospital Corporation of America, are skin irritants such as, wool or synthetic clothing; soaps or detergents; cosmetics or perfumes; dust/sand; chemical solvents; and chlorine. Some other environmental factors could be extremes in temperature/climate or lack of moisturizing after a bath.
According to the Mayo Clinic, eczema is a chronic condition and because of that, there is no permanent cure. Although there are no permanents cures, there are treatments to help the symptoms of eczema.
In an email to SciJourner, Robert Sidbury, Professor in the Department of Pediatrics at the University of Washington School of Medicine, said that the best treatments depend on the severity. According to Sidbury, “A foundational treatment for all eczema is simply moisturizing the skin.”
Moisturizing the skin helps keep the water in and keeps allergens and infectious agents (something that infiltrates another living thing) such as, staph bacteria and herpes complex out. Staph bacteria is related to eczema because it is commonly found on the skin. Herpes complex is related to eczema because people who have it can go through periods of attacks(outbreaks).
Although moisturizing the skin is helpful for most eczema diagnosed patients, it may not be enough for all. I moisturize and it seems to help plenty. Patients with a more moderate type of eczema may use anti-inflammatory agents, like topical steroids, topical calcineurin inhibitors, or the more current topical phosphodiesterase.
Sidbury stated, “Topical therapy (e.g. creams, ointments, lotions, oils) are not sufficient for the more severe end of the eczema spectrum.” For these patients, systemic (oral, injectable, phototherapy, etc.) treatment is required.
According to the NEA, the most commonly prescribed medication for all types of eczema is topical corticosteroids, or just “steroids.” Some side effects from using steroids are: skin thinning, stretch marks, easy bruising/tearing, and enlarged blood vessels. Although I use a topical steroid ointment, I have yet to experience any of these side effects.
Now, my eczema is better. Although my skin is still sensitive, it is clear and smooth, unlike when I was younger. I continue to use my prescribed medicine whenever I get eczema flare-ups, but that has not been the case for a while.

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License.

By Tiziana Zappone and Michel Garcia; Farnsley Middle School (Louisville, KY)
“I had headaches and I would hear buzzing in my ears,” said Robert Peña Hernandez (co-author Tiziana’s dad). “I would have never thought it was high blood pressure. I went to the doctor in August because I had a stuffed-up ear. I expected the doctor to tell me I had a minor ear infection, but instead the doctor told me I had high blood pressure.”
According to the American Heart Association (AHA), “High blood pressure (HBP or hypertension) is when your blood pressure, the force of the blood flowing through your blood vessels, is consistently too high.”
High blood pressure is also known as the “silent killer”, because there are no detectable symptoms. However, if left unattended there is a possible chance of having a heart attack, stroke, or other health threats.
According to the AHA, the only way to diagnose HBP is to have your blood pressure taken.”
Blood pressure numbers look like fractions. The numerator (upper number) is the systolic blood pressure. As reported by the Centers for Disease Control and Prevention (CDC), “the first number, called systolic blood pressure, measures the pressure in your blood vessels when your heart beats. The second number, called diastolic blood pressure, measures the pressure in your blood vessels when your heart rests between beats.” ͖The diastolic blood pressure is the denominator (lower number). Blood pressure is measured in millimeters of mercury (mm Hg). A normal blood pressure is less than 120/80. An elevated blood pressure is 120-129/80 or more. The first stage in HBP is 130-139/80-89. The second stage in HBP is 140 or higher/90 or higher. To be in hypertensive crisis, you have to have 180 or higher/120 or higher. Peña Hernandez thinks his numbers were 185/130.
There is a higher chance of developing hypertension if you’ve had thyroid or kidney problems. The Mayo Clinic states that the older you are, the higher chance you have of having high blood pressure. Being overweight or obese is also a risk factor. This is because the more you weigh, the more blood you need to supply oxygen and nutrients to your tissues. The pressure of your artery walls increases as well as the volume of blood circulating in your blood vessels. Another risk factor is family history.
Peña Hernandez could’ve developed hypertension because his father also has it.
WebMD stated that there are medications to help treat high blood pressure, but they cannot cure it. Some of the medications include lisinopril oral, atenolol oral, bystolic oral, diovan oral, hydrochlorothiazide oral, and amlodipine oral.
Peña Hernandez is taking one of the medications called lisinopril, given to him as a prescription drug by his doctor. According to everydayhealth.com, a site that is committed to providing health and medical information from healthcare providers, “It works by widening blood vessels, which allows blood to flow more smoothly and lets the heart function more efficiently.”
One of the main side effects of lisinopril is continuous coughing, which is the only side effect Peña Hernandez had when taking lisinopril. Because of his coughing, Peña Hernandez’s doctor prescribed him LOSARTAN/ HCTZ, which he takes every day after he gets home from work.
Peña Hernandez is currently in a healthy condition and has a lower blood pressure than before. His blood pressure is usually 120/90 when he takes his medication. “I don’t cough as much as I did before and my blood pressure has lowered.”

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License.