By Aniket P Patel and Anthony Cruz; Farnsley Middle School (Louisville, KY)
“I was having pain in the bottom part of my right back and I couldn’t breathe,” Peter Patel (Aniket’s Dad) stated. “I just thought it was back pain and left it alone thinking it will be fixed in a week or two.”
However, the pain continued at night and it got worse. He said he was having problems breathing so Aniket’s mom took him to the hospital on March 19, 2017. After two CT scans, the doctors said that he had a lung abscess. He had infection in the top half of his right lung that caused fluids to get stuck in the bottom part of the lung. The whole right side of his lung was not working. That’s why he was having problems breathing.
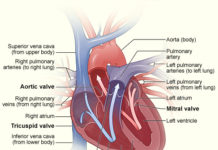
The cause of his infection was a bacterium called Streptococcus intermedius. According to National Center for Biotechnology Information (NCBI), S. intermedius is a member of the Streptococcus anginosus group. It usually lives in the brain, meninges, heart, sinuses, liver, lungs, spleen, peritoneum, pelvis, and appendixes. Sixty-five percent of these infections are produced by anaerobes so it’s easier for them to grow in these places because there is no air. It causes abscesses and fluid, clogging the organ where ever it grows.
According to Centers for Disease Control (CDC), research shows that more likely people from India are affected by this bacterium. Other races are affected, but less so.
A lung abscess is when infection—most of the time caused by bacteria or fungus—spreads throughout the lung tissue. This causes fluids to get trapped in the lungs and makes it harder to breathe. Also sometimes called necrotizing pneumonia, the infection is usually bigger than 2 cm in radius, and can spread to your whole lungs, as stated by Wikipedia.
Patel was lucky that he only had it the right side of his lungs.

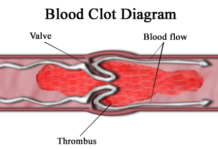
According to NCBI, there are several ways bacteria can get into your lungs. Haematogenous, which means originated in or carried by blood, is one way and bronchogenic, which means originated in your lungs, is a second way that bacteria. Sometimes, these bacteria can also get in through inhalation and through food. When these bacteria arrive in the lungs they are attacked by cells called phagocytes, which then release chemicals that fill your lungs and kill some parts of lung tissues, as well.
The symptoms of lung abscess include coughing up blood or pus-like material with a bad smell, bad breath, a fever of 101 °F or higher, chills, chest pain, shortness of breath, sweating or night sweats, weight loss, and fatigue, as stated by NCBI. Patel’s symptoms were shortness of breath, chest pain, fever of 101 °F or higher, chills, and sweating at night.
According to healthline.com, people who are alcoholic or have recently been sick have a higher chance of lung abscess. Also, people with weak immune systems or have conditions, such as cancer, HIV infection, organ transplant, or autoimmune disease. The risk is pretty high even for people who have recently been under anesthesia, sedation, or unconsciousness from injury. However, Patel didn’t have any of these problems.
Also, according to healthline.com, a lung abscess is mostly detected by CT scans and X-rays to find the infection and fluids. It can also be determined that you have a lung abscess by your health records. There is pain in the chest, problems breathing, and just a little bit of burning at the infection site.
The Mayo Clinic states that a lung abscess can be treated by different kinds of antibiotics, such as Clindamycin 600 mg in IV, metronidazole 500 mg tablets, amoxicillin/clavulanate875/125 mg in IV, clindamycin 300 mg, and vancomycin or linezolid.
Patel’s doctor prescribed AMOX-CLAV 500MG TABLETS a generic form of AUGMENTIN 500MG TABLETS. You must take the medicine for 3-6 months as directed by the doctor. In some cases, where the fluid is stuck, surgery is required. Tubes are entered through your ribs into your lungs where the fluids are. The fluids are sucked up to open the lungs and be able to breathe.
Patel was able to breathe perfectly fine 15 days after his tubes were taken out. The infection is still healing and may take up to 3 months to be completely free from the infection.
“I never want to have any problems like that again,” he states. “It just burned in my lungs and I thought it was just back pain. Now I can breathe fine and it doesn’t burn anymore in my lungs.”

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License.











A really interesting and informative article, especially with the current wave of respiratory ailments. Timely and relevant. Nice work!