Open fetal surgery—a radical, new approach to treat the most severe form of spina bifida—has proven to be a successful treatment for this dangerous condition, according to a clinical study published in the March, 2011, issue of the New England Journal of Medicine. The open fetal surgery corrected a type of spina bifida called myelomeningocele, the most common form of the birth defect, which results in the spinal cord being open on the back of the fetus.

According to the Spina Bifida Association, spina bifida occurs when the spine does not close all the way as the fetus is developing in the womb. In the United States, about 1,500 to 2,000 babies are born each year with spina bifida, according to the National Institutes of Neurological Disorders and Stroke.
Spina Bifida is one of the most common physically disabling birth defects and usually occurs early in pregnancy. According to the National Institutes of Health, spina bifida usually leads to paralysis of the legs, which requires the assistance of braces, crutches or wheelchairs. Children with spina bifida may also have learning difficulties, urinary and bowel problems, and a potentially fatal build-up of fluid on the brain—a condition known as hydrocephalus.
In the past, treatment for myelomeningocele required surgery within a few days of birth. Open fetal surgery was typically only used for life threatening defects. In recent years, however, doctors have begun using open fetal surgery to treat myelomeningocele while the fetus is still developing, a technique pioneered at Vanderbilt University Medical Center. In open fetal surgery, the mother is given general anesthesia and the uterus is opened, allowing doctors to work directly on the fetus. After the surgery, the fetus is returned to the uterus to continue developing until delivery.
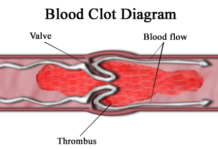
The results published in the New England Journal of Medicine came from MOMS—the Management of Myelomeningocele Study. MOMS, which began in 2003 and included 158 subjects, compared outcomes of fetal surgery with postnatal surgery. The results showed that fetal surgery reduces the need to divert fluid away from the brain, a process known as shunting. MOMS also showed that the children had improved motor function and mental development, as well as increased odds of walking unassisted. Closing the fetus’s spinal column in utero may actually reverse the development of myelomeningocele by allowing some nerve function to be restored throughout the rest of the pregnancy, say the researchers. Open fetal surgery was considered successful enough that the clinical trials were stopped early so that those scheduled to have surgery after delivery could have access to fetal surgery instead.
Open fetal surgery is not without risks. Recipients of open fetal surgery were more likely to be born several weeks earlier than the postnatal group. On average, they were born after 34 weeks of pregnancy compared to 37 weeks for the postnatal group. However, there was no difference in cognitive development. Other risks include thinning or tearing at the women's surgical incisions requiring Caesarean sections for later births.
Despite the risks, many parents consider open fetal surgery a viable option to improve their child's quality of life. "The experts we met with locally (a perinatologist and a pediatric neurologist) both felt strongly that the fetal surgery could help with the hydrocephalus aspect of Spina Bifida,” wrote Sara Zimmerman, a mother of five and a participant in the trial. Zimmerman blogged about her experiences and continues to write about raising her daughter, Ruth, who has spina bifida. “She does not have a shunt, but she may still need a shunt. She may not walk without braces, but it looks promising as she has great movement and strength in her legs. She already has issues with her bladder and kidneys, and requires medication and cathing. Is she better off because of the fetal surgery? I believe so.”
Edmund Yang, now a professor at Saint Louis University School of Medicine, was the principal investigator of the MOMS Trial at Vanderbilt University. Yang now heads the St. Louis Fetal Care Institute, a division of Cardinal Glennon Children’s Medical Center, which is only one of eight in the nation to offer open fetal surgery. The first surgery to treat myelomeningocele in St. Louis was performed on May 20, 2011. "A lot of families just can't afford to get the best care because it's not in their location," said Yang in a press release in 2009 when the St. Louis Fetal Care Institute first opened. "We're ready to take care of these families in St. Louis."

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License











An outstanding article. I especially appreciated how you described spina bifida so clearly and simply for readers like me. Also, you provided really helpful context for me to better understand the significance of the MOMS study. Well done!